Penicillin Allergy: What You Need to Know Before Avoiding Antibiotics
Many people worry they are “allergic” to penicillin, but most who carry that label are not truly allergic and can actually take penicillin safely after proper evaluation. Understanding what a real penicillin allergy is, how to get tested, and when to avoid penicillin can help you and your clinician choose the safest and most effective antibiotics.
How common is penicillin allergy, really?
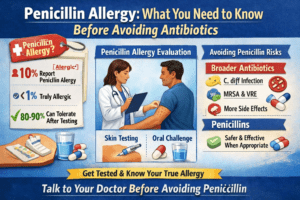
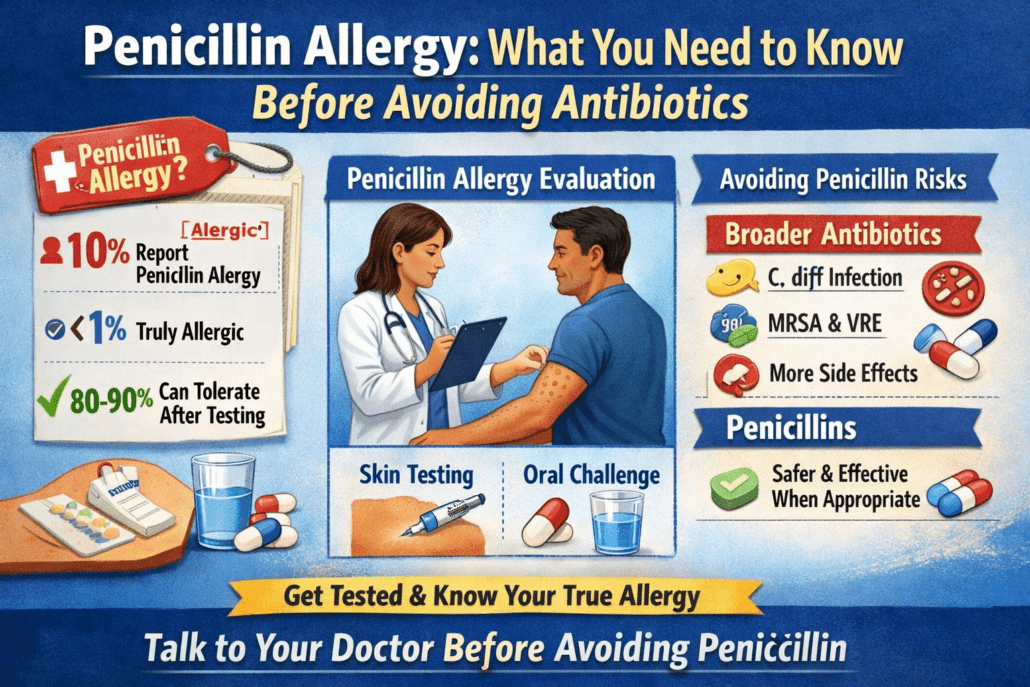
- About 10% of people in the United States say they have a penicillin allergy.
- When those patients are formally evaluated, fewer than 1% of the total population are found to be truly allergic.
- Studies show that 80% to 90% of people once labeled penicillin‑allergic can ultimately tolerate penicillin again, especially if many years have passed.
In practice, this means many penicillin “allergies” are inaccurate labels, often based on childhood rashes, side effects like stomach upset, or vague memories of a reaction. Losing this label when it is not accurate is important because it opens the door to better, narrower‑spectrum antibiotics and fewer complications.
Why does the label matter?
Carrying a penicillin allergy label affects more than just one prescription.
- You are more likely to receive broad‑spectrum antibiotics like fluoroquinolones, clindamycin, or vancomycin instead of first‑line penicillins.
- Use of these broader drugs is linked with higher rates of C. difficile infection, MRSA, and VRE, as well as more drug side effects.
- People with a penicillin allergy label may have longer hospital stays, more surgical site infections, and higher healthcare costs.
Because of these risks, allergy and infectious disease experts now strongly encourage proactively evaluating penicillin allergy labels rather than avoiding penicillin for life.
Example
A patient labeled “penicillin‑allergic” as a child for a mild rash later needs surgery. Instead of a standard penicillin‑type antibiotic, they receive a broader drug and end up with C. difficile diarrhea, a complication that might have been avoidable if their label had been checked and removed.
What does a true penicillin allergy look like?
A true penicillin allergy is an abnormal immune reaction to the drug, and it can be immediate (within minutes to hours) or delayed (days later).
Immediate (IgE‑mediated) reactions
These usually occur within an hour but can show up within the same day of a dose. Common features include:
- Hives (raised, itchy welts)
- Swelling of lips, tongue, face, or throat
- Trouble breathing, wheezing, chest tightness
- Dizziness, fainting, low blood pressure
- Anaphylaxis, which is a life‑threatening whole‑body allergic reaction
Immediate allergic reactions are serious and require urgent care; patients with this pattern should avoid penicillin until evaluated by an allergy specialist.
Delayed reactions
Delayed reactions show up days after starting penicillin and can range from mild to life‑threatening.
- Mild: flat red rash, sometimes itchy, without other symptoms.
- Severe: syndromes such as Stevens–Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), drug rash with eosinophilia and systemic symptoms (DRESS), and other organ‑involving reactions.
If you have ever had a severe delayed reaction like SJS, TEN, or DRESS, you should never take penicillin or undergo penicillin challenge testing again.
What is not a true allergy?
Many reactions blamed on penicillin are not immune allergies at all. Examples include:
- Nausea, vomiting, or diarrhea without other symptoms
- Headache or fatigue
- Yeast infections after antibiotics
- A viral rash that happened to appear while taking penicillin
- A family history of penicillin allergy without any reaction yourself
These situations often can be “delabeled” simply by reviewing your history with a clinician, sometimes backed up by a supervised single‑dose challenge.
How can I find out if I am really allergic?
National allergy organizations recommend that penicillin allergy evaluations be offered proactively, even before you need antibiotics. This can usually be done in three steps.
- Detailed history
Your clinician or allergist will ask about:
- What penicillin drug you took (for example, amoxicillin)
- What happened, including your symptoms
- How long after taking the dose the symptoms started
- How many years ago this occurred
- Whether you have taken any penicillin‑type or cephalosporin antibiotics since then without issues
Many people with only vague, mild, or very remote skin‑only reactions (more than five years ago) are considered “low risk.”
- Skin testing (when needed)
For patients with a higher‑risk history — like hives, wheezing, or a concerning recent reaction — penicillin skin testing is often recommended.
- Small amounts of penicillin test reagents are placed on or just under the skin.
- The allergist watches for a localized hive reaction that suggests allergy.
- If skin testing is negative, the next step is usually an oral challenge.
Penicillin skin testing has a very high negative predictive value, meaning that if your test is negative and you pass an oral challenge, your risk of an allergy reaction is similar to someone with no history at all.
- Direct oral challenge
For many low‑risk patients, guidelines now support a direct supervised oral challenge with a penicillin such as amoxicillin, sometimes without prior skin testing.
- You take a small dose under observation, then a full dose if there is no reaction.
- Staff monitor you for a set period for any signs of allergy.
- If you tolerate it, the penicillin allergy label can usually be removed from your chart.
People with a history of severe delayed reactions (SJS, TEN, DRESS, severe organ injury) should not undergo this kind of challenge.
If my test is negative, is it safe to use penicillin?
When skin testing (if done) and an oral challenge are negative, you can typically use penicillin and related antibiotics when needed. Research shows that these patients do not have a higher risk of immediate IgE‑mediated reactions than the general population.
It is important to have your medical records updated to remove the penicillin allergy label and document your testing results clearly so the allergy is not accidentally re‑added in the future.
What if I truly am allergic and need penicillin?
Sometimes penicillin is the only recommended treatment, such as for neurosyphilis or syphilis in pregnancy. If you have a confirmed penicillin allergy and no good alternative antibiotic:
- You may undergo a process called desensitization in a monitored hospital setting.
- Tiny, gradually increasing doses of penicillin are given over hours until the full dose is reached.
- This temporarily trains your immune system to tolerate the drug so the course can be completed safely.
Desensitization does not “cure” the allergy permanently, so you should continue to be labeled allergic unless retested and advised otherwise by an allergist.
When should I talk to a doctor about penicillin allergy?
You should seek medical advice if:
- You have a penicillin allergy label but do not clearly remember the reaction.
- Your reaction happened in childhood or more than five to ten years ago.
- Your reaction was just stomach upset, a mild rash, or a family history.
- You are pregnant or planning surgery and carry a penicillin allergy label.
- You have had a concerning reaction such as hives, wheezing, swelling, or feeling faint after penicillin.
An allergist or knowledgeable clinician can help decide whether you should be delabeled by history, undergo a supervised oral challenge, have formal skin testing, or continue to avoid penicillin. Early evaluation — before you urgently need antibiotics — gives you more options and time to make a safe plan.
If you carry a penicillin allergy label or are unsure about a past reaction, schedule an appointment with us today to review your history and discuss testing options so you can safely expand your future antibiotic choices.
Sources
- CDC – Clinical Features of Penicillin Allergy (Antibiotic Prescribing and Use)
- StatPearls – Penicillin Allergy (NCBI Bookshelf)
- AAAAI – Penicillin Allergy evaluation/position statement and public guidance (American Academy of Allergy, Asthma & Immunology

 Claire is an American Academy of Nurse Practitioners board certified Family Nurse Practitioner with a special interest in allergy and immunology. She is a summa cum laude graduate of Providence College where she received her Bachelor of Science in Biology. She then went on to receive her BSN and MSN from MGH Institute of Health Professions and has been working as a Nurse Practitioner in Allergy ever since.
Claire is an American Academy of Nurse Practitioners board certified Family Nurse Practitioner with a special interest in allergy and immunology. She is a summa cum laude graduate of Providence College where she received her Bachelor of Science in Biology. She then went on to receive her BSN and MSN from MGH Institute of Health Professions and has been working as a Nurse Practitioner in Allergy ever since.